read pdf version
read pdf version
Presentation to SALT, September 11 2007: Privatizing Continuing
Care
The continuing care system is, theoretically, a continuum of services from home
care
through supportive living, and continuing care centres. There are variations
in the care
that's provided within each bit of the system, but generally speaking, each
level provides a
higher level of care. It's been an evolution over 50 years, from auxiliary hospital,
nursing
home, senior lodges, and home care, provided by a variety of operators with
a high rate of
public funding for the health care services and with housing cost subsidies.
At various times along the way, particularly in 1982 with the Alberta Nursing
Home Review
Panel (Hyde) Report , and the 1988 A New Vision for Long Term Care, recommendations
were made to rationalize the system, including integrating the services under
a proposed
Long Term Care Act, and developing more "community based" options for providing
housing
and support services.
The auxiliary hospital and nursing home services were merged, reducing the skilled
nursing
care and rehabilitation services, and the "single point of entry" system was
initiated. New
services began to emerge: personal care services in private and group homes,
specialized
dementia care programs, assisted living, and day programs which coordinated
a variety of
care services. There were also "transition" programs, primarily to provide short-term
care to
reduce the pressure on acute care hospitals, often located in continuing care
facilities. The
underlying issues were both increasing demands for services, and a change in
philosophy
from institutional medical care to a community-based provision of services.
The subtext in these policy developments was that health care in general (and
particularly
for old folks, whose numbers were increasing) was costing a lot of public money.
That
became the primary message in the mid-90s. Both care facility and home care
services
were cut and downgraded, unbundling and delisting shifted costs to the users,
and seniors'
benefits were cut. Responsibility for providing services was shifted to the
regional health
authorities (under the direction of Alberta Health). The funding model changed
from a
program basis to a global population model, increasingly distanced from assessments
of
care needs. And we must not forget the famous Taft report from the early 1990s,
which was
shredded because its findings did not support government Policy that seniors
care costs
were escalating out of control. (Kevin Taft was also involved in the 1982 Hyde
report, which
identified a number of concerns about quality of care and funding.)
The Broda reports (1999 -2002) and related health care policy initiatives redefined
the
public role in continuing care services. Government responsibility for health
care was
redefined from direct service provider to setting strategic direction for the
system through
policy, legislation and standards; allocating resources; helping develop and
support the
health system; and administering provincial programs. Government would no longer
be
involved in building new housing facilities - from 1959 to 1993, government
funded the
construction of senior citizens' homes.
Beginning in 1994, in recognition that public subsidies were necessary to support
private
capital investment, capital funding was made available to non-profit organizations
to develop
new seniors' housing. By 2003, this funding was also available to private for-profit
developers. Both for-profit and not-for-profit care centre operators have had
access to
pubic funding for construction costs, renovation and with the operating contracts;
these
subsidies are now being extended to supportive living facilities.
There has not been a consolidated report of the public funding for continuing care facilities.
I did find, in the ASCHA newsletters, a list of 2005/07 recent Rural Affordable Supportive
Living capital grants to 17 private for-profit care facility operators which totaled $16.5 million.
RASL is only one of the capital funding programs available. When you see a press release
announcing "Provincial surplus helps create more housing in rural Alberta", you need to look
at the "Backgrounder" to discover, for example, that we're paying $2.4 million for half the
construction costs of a Continuum Health Care Holdings Ltd. project under the Rural Capital
Projects Initiative, which will be supported by a long term operating contract with the health
region, and undoubtedly made more profitable by deals with land purchase and other perks.
The number of care spaces available is really hard to determine. Historical data reports
12,982 long term residents in 1990. From 1997 to 2003, Alberta Health published an
annual census of long term care residents, including care needs classifications; these
number show an increase from 12,836 in 1997 to14,449 in 2003. These numbers don't
coincide with other reported numbers (for instance, the RHA funding manual [2005/06]
reports 12,732 residents in 2003). When Alberta Health was asked to reconcile the differing
numbers, they said the resident count for 2003 was 12,940 and for 2006, 12,551. But
there can be no doubt that significant numbers of folks are being shifted to assisted and
supportive living settings, which are increasingly privately owned and operated.
In 1990, Alberta's population was 2.5 million; in 2000, 2.9 million, and by 2006, 3.4 million.
Assuming the same proportion of the population (about 0.5%) need serious long term care,
the care facility resident population should have increased at the same rate. But we know
that seniors are now a somewhat larger proportion of the population, and that those with
serious and complex health problems are living longer.
There is also no doubt that increasing numbers of people who apply for continuing care
(including home care) are not being assessed for care which coincides with real life needs.
The assessment criteria have traditionally been adjusted downward when the wait lists get
out of control, assessed needs have more to do with services provided than with individual
needs, and it's all relative, anyway; the wait lists were cut in half when the "waiting in the
community" category was dropped. If you're not "urgent", you can wait until you are. Or,
you can buy private care, often in the same facilities that have contracts with the health
regions for "designated" spaces.
At Columbia Assisted Living, in Lethbridge, personal care services may be provided by the
RHA Homecare Program, and are also available from their staff. Rent, for one person is
$1585 or $1895/month (plus telephone and cable). (Laundry is probably coin-operated.)
Laundry Service (once a week)
$35.00 per month
Bath - 30 minutes
$9.00 per bath, or
1 per week
$36.00 per month
Dressing (AM or PM) - 15 minutes per
$135.00 per month, or
Dressing (AM and PM) - 15 minutes per
$270.00 per month for both
Feeding - 20 minutes x 3 daily
$360.00 per month
Medication Management
$50.00 per month
Mobility (to dining room/return x 3 daily)
$270.00 per month
Toileting - 10 minutes
$90.00 per month
Full personal care services offered: $1111
Page 2 of 6
At Holy Cross Manor in Calgary, even higher rents were raised earlier this year by 40%.
The last posted "Available Optional" service charges (subject to GST) were:
ADDITIONAL OCCUPANT CARE SERVICES AND MEALS FEES:
$750.00
MEDICATION ASSISTANCE PROGRAM:
$300.00
MEDICATION REMINDER:
$175.00
RESIDENT NIGHT CHECKS:
$175.00
FT MEAL ESCORT: (3 meals/day 7 days/week)
$300.00
PT MEAL ESCORT: (2 or less/day 7 days/week)
$175.00
DAILY TRAY SERVICE:
$300.00
MEAL TIME REMINDER:
$175.00
DAILY LIGHT HOUSEKEEPING:
$300.00
WEEKLY PERSONAL LAUNDRY SERVICE:
$50.00
SUPPORT STOCKING ASSISTANCE:
$250.00
INCONTINENCE MANAGEMENT:
$300.00
EXTRA ASSISTANCE:
$350.00
BATH ASSIST X 1(ONE/WEEK):
$100.00
BATH ASSIST X 2(TWICE/WEEK):
$175.00
RESIDENT PARKING PER VEHICLE:
$100.00
SHAW BASIC CABLE PACKAGE/month
$20.00
Full personal care services offered: $2200
Current government care rates to operators for "designated" residents" are:
Assisted Living (2hrs. unscheduled care), $47.50
Enhanced Assisted Living (3 hrs unscheduled care), $72
Facility care, $148
The trend is to replace facility care with supportive living options. The distinctions are no
longer clear; the initial justification was to delay or avoid "institutional care" as long as
possible. But while the new assisted and supportive living facilities may be more attractive
than a care centre built a decade or more ago, they are still a residential care facility. The
difference is the level of care, and the competencies of the care staff and the cost.
When Phil Gaudet (President and CEO of the Good Samaritan Society) said that assisted
living might be seen as a "dumbed-down" care facility in 2002 , he was also in the process of
selling the concept of assisted living facilities to replace care facilities. Good Sam has
subsequently greatly expanded its assisted living operations in British Columbia and Alberta,
with bundles of capital grant money. The Good Sam subsequently converted their publicly-
funded Hinton care facility to a Designated Assisted Living facility, with financial help from
the Aspen Health Region.
The shift to "community care" and the "unbundling" of care services has market opportunities
for private providers (I've seen a number of advertisements for home care service provider
franchises, some of which are operating in Alberta). The ownership of operators is difficult
to trace; most appear to be Alberta or Canadian owned, but it is possible that some may be
connected with American health care providers.
Page 3 of 6
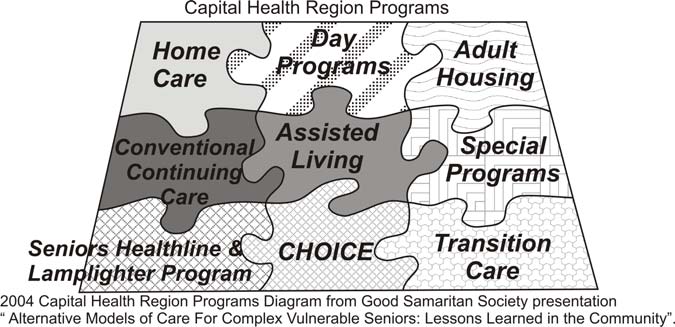
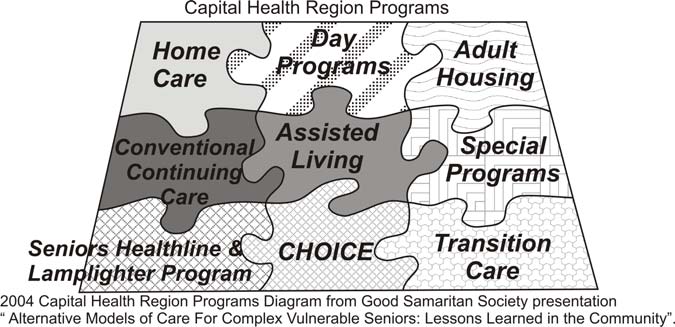
(CHOICE = Comprehensive Home Option Integrated Care of Elderly)
One of the persistent problems with tracking what's happening, or identifying issues,
is the absence of information; this is an issue of both accountability and of
transparency and even of competence. Quite simply, Alberta Health frequently
responds to requests for information by saying "we don't track that" or "the health
region reporting data in not consistent (or comparable)", or "the details aren't
reported". Ask the health regions for information, and they refer you to a FOIP
application and the fees.
The extent of the private market opportunities is enormous. There's been a new interest in
"Corporate Memberships" of both the Alberta Senior Citizens Housing Association (ASCHA)
and the Alberta Continuing Care Association (ACCA, formerly the Alberta Long Term Care
Association), lobby groups for the operators. (For $1500 a year, corporate members get to
advertise products and services (including staffing agencies, home care services, long term
care insurance, pharmaceuticals, energy, food services and management agencies) to the
industry, attend meetings (but not vote), and also enjoy the benefits of "Government
Liaison". Many of these suppliers are subsidiaries of facility operators already represented.
The Mission Statement of the ACCA, in 2005, was "To provide the best available
information and services to our members and continue to work with the government
of Alberta to improve legislation that affects long term care as a growing industry".
It's been rewritten, to "Enhancing quality of life for individuals receiving continuing
care by assisting members in networking, advocacy, education and pursuit of best
practices".
There is also a great deal of investment by international investment banks in the "retirement
living" market. We're not just dealing with Summit Care Corporation, an Alberta company
(which may or may not be affiliated with Summit Care Corporation US), or Columbia Health
Care (with equally suggestive associations), or Extendicare, which operates infamously in
the US. Central Park Lodges, a Canadian health care services company previously owned
by the Reichmanns, became CPL REIT and then Retirement Residences Real Estate
Investment Trust, which also operates in the US and was chaired at one time by one
William G. Davis, with Ernie Eves as a Board member.
(See attached extract from 1997 Prospectus).
The Macquarie Bank is another player: in addition to the Toronto 407 toll road, a share in
AltaLink (chaired by David Tuer, also Chair of the Calgary Health Region), and Cardinal
Page 4 of 6
Power, they also own Leisureworld (and retirement care operations in other countries).
Leisureworld operates retirement communities, independent living facilities, assisted living
facilities, and nursing homes; the purchase included Preferred Health Care Services, which
provides staff for care facilities and for private care.
Aged Care a growth industry for Investors discussed why the resident fees have increased;
the plan was first publicly outlined in the Broda report's final recommendations:
Recommendation 23 Adopt a conceptual framework on responsibility for costs: The
conceptual framework should be adopted as the basis for decisions about responsibility for
the costs of different types of continuing care.
Who is responsible for the costs of continuing care?
Cost components
Home care
Supportive living
Long term care facility
Professional care, e.g.
Government 100%
Government 100%
Government 100%
health and medical
treatments, visits, tests,
etc.
Activities of daily living,
Government/individual
Government/individual
Government/individual
e.g. personal care and
share costs
share costs
share costs
homemaking services
Accommodation, e.g.
Individual 100%
Individual 100%
Individual 100%
food, cleaning, utilities,
etc.
Capital, e.g.
Individual 100%
Individual, with income
Shared responsibility:
construction, renovations
support where needed
Individual 33%
and upgrading
(through rental
payments) Owner 33%
Government 33%
What I didn't say in that paper was that, given occasional expressions of concern by private
operators that they don't have a level playing field when they have to compete with public
services16, both the fee increase to reach "full cost recovery" and the capital subsidies to
private operators were inevitable. There is already confusion about which "envelope" care
staff is paid from; the "blended jobs " really confuse the line between health care, personal
care, and housekeeping. That will probably be next. And then there was Recommendation
25: Additional revenues raised from increasing charges for residents of continuing care
centres should be used in two ways:
§ Improving services in continuing care centres. . .
§ Establishing a capital pool to be used in each region to renovate and build new
continuing care centres The remaining portion should be used to upgrade facilities.
Is assisted living cheaper? We don't know. There's concern that the studies claiming to
show it's less expensive don't count all the costs, or comparable costs; and there is the
caveat that the costing doesn't include the out-of-pocket costs to the resident, which often
include medications, supplies and equipment, and supplementary care staff. We don't
have any idea what the cost of deferred capital funding from the grants will be.
Administrative costs probably don't include the costs of the contracting processes, and
certainly the profits (or, in the case of non-profit organizations, the "investment fund") aren't
identified.
Is assisted living better? For some folks, it's the cat's pajamas. For many, it's too
expensive. And for some it's purgatory. But it is not public health care.
Page 5 of 6
What's the government doing next?
The Health Service Standards have been incorporated into the Nursing Home Regulations,
and Alberta Health is in the initial stages of developing a Compliance Unit. The Standards,
of course, are simply process statements for required policy development, which the health
regions will include in service contracts. They don't apply to services privately provided
which means, in a facility where some spaces are "designated" and some are private, or if
you buy private home or nursing care, you're on your own.
The Supportive Living Accommodation Standards present a different problem. I wrote a
short article (in the handouts) with my concerns about the current initiative to develop them
into Supportive Living Accommodation Standards and Licensing (proposed for next spring).
In the first place, the standards don't include ordinary consumer tenancy protection. Similar
legislation in B.C. has clearly not worked for tenants. But at bottom, what it will do is write
the separation of housing and health care for vulnerable seniors into law.
Premier Stelmach has proudly been talking about the Lobbyist Act so we'll know who's
trying to influence public policy and decision-makers. The Muttart Foundation and Volunteer
Alberta have initiated a lobby to exclude non-profit organizations from this registry. We
know that the care facility and seniors' housing operators, and their associations, have been
heavily involved with lobbying for the changes we've seen to continuing care.
We know that both the ACCA and ASCHA have been represented on Government
committees: Broda had Carl Bond, owner of Summit Care Corporation and Travois
Holdings and (then) President of the ALTCA; the legislative review committee for
the Protection for Persons in Care Act had Carl Bond, Greer Black, president of
Bethany Care Society and currently President of the ACCA; and Lyn Krutzfeldt,
director of Central Park Lodge for Western Canada and also then a member of the
Capital Health Authority Finance Committee and the Capital Health Peer Review
Committee. We know that the Alberta Senior Citizens Housing Association and the
Alberta Continuing Care Association were given funds to develop the Standards and
are part of the ongoing Departmental review and implementation committees.
I've been trying to differentiate between the business of Extendicare and The Good
Samaritan Society, to see how they differ so that the lobby efforts Good Sam should be
excluded from even this public scrutiny. The only difference I can see is the professed
religious beliefs of the Boards. I think this is worth public discussion, and perhaps even a
presentation to the policy field committee.
What needs to be done? That's what I hope we can talk about. There aren't any easy
answers, but there is urgency.
Carol Wodak, September 11, 2007
Page 6 of 6
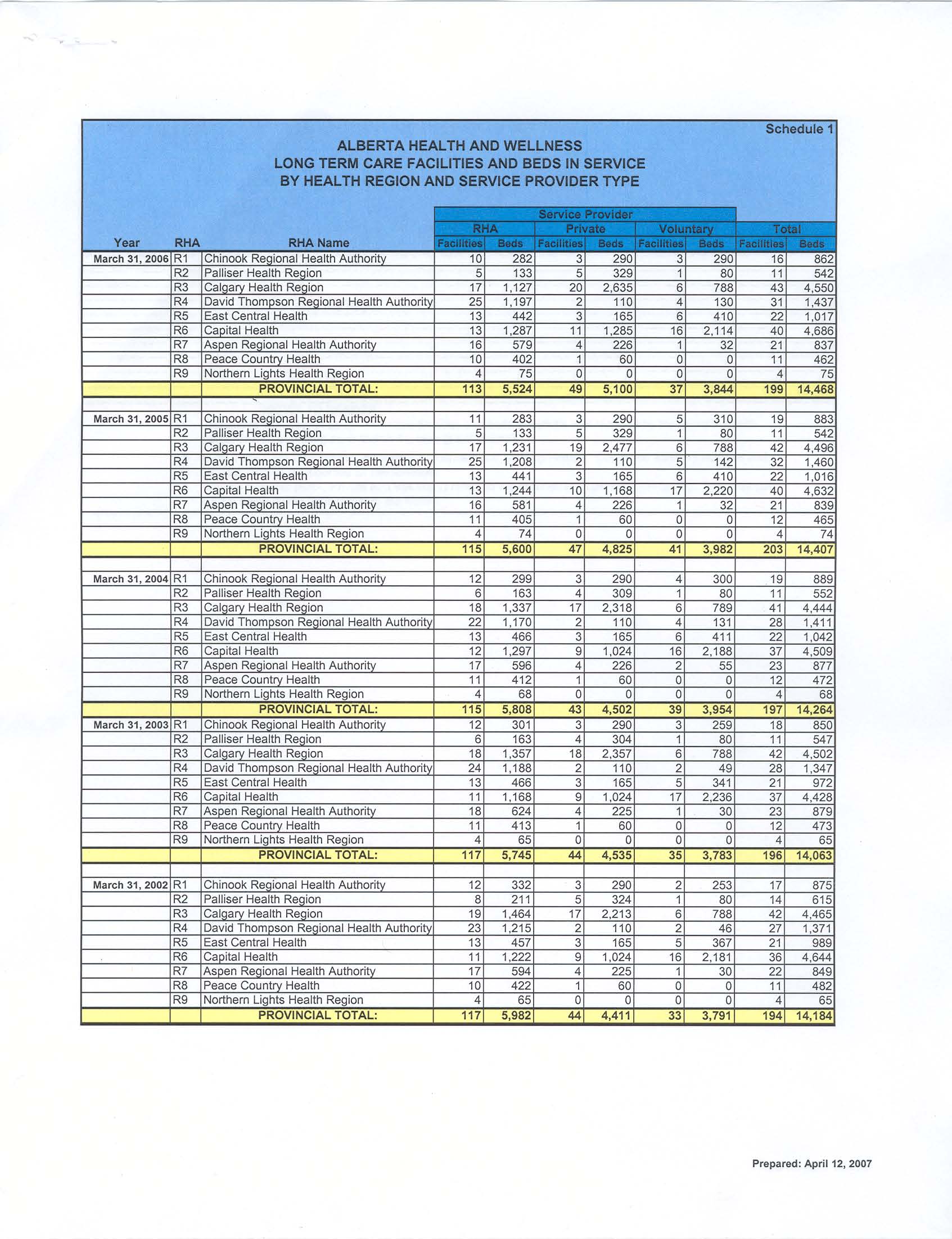
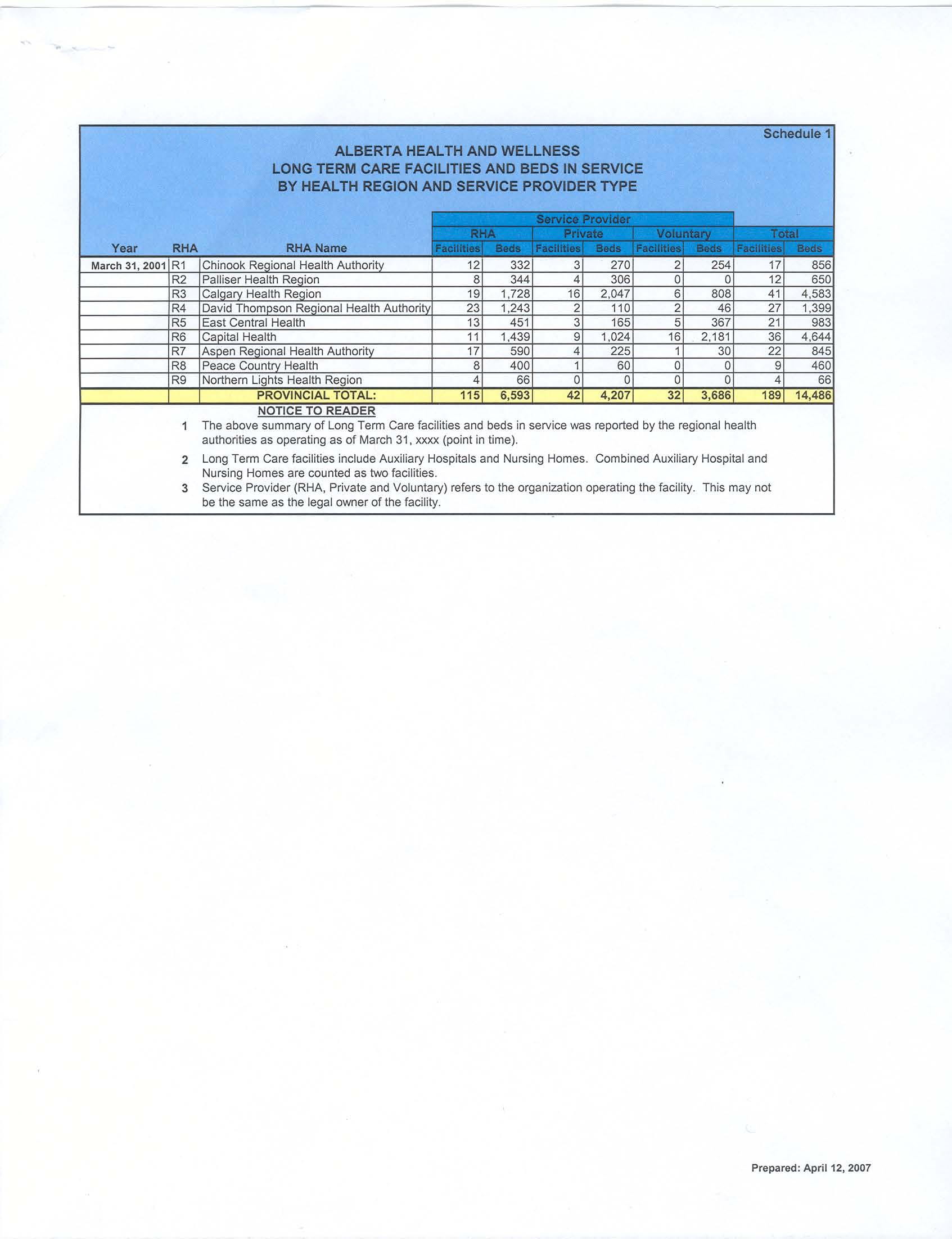
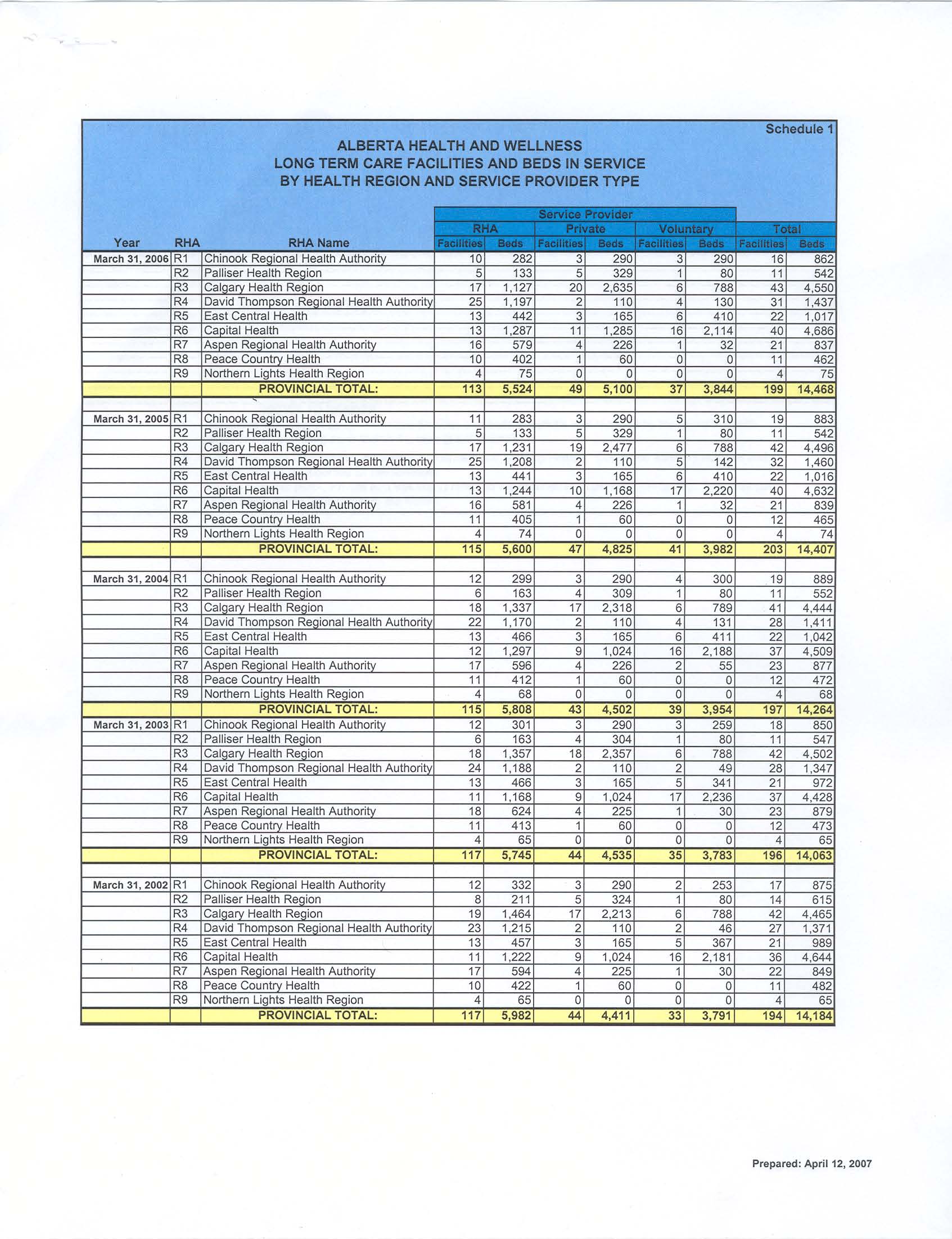
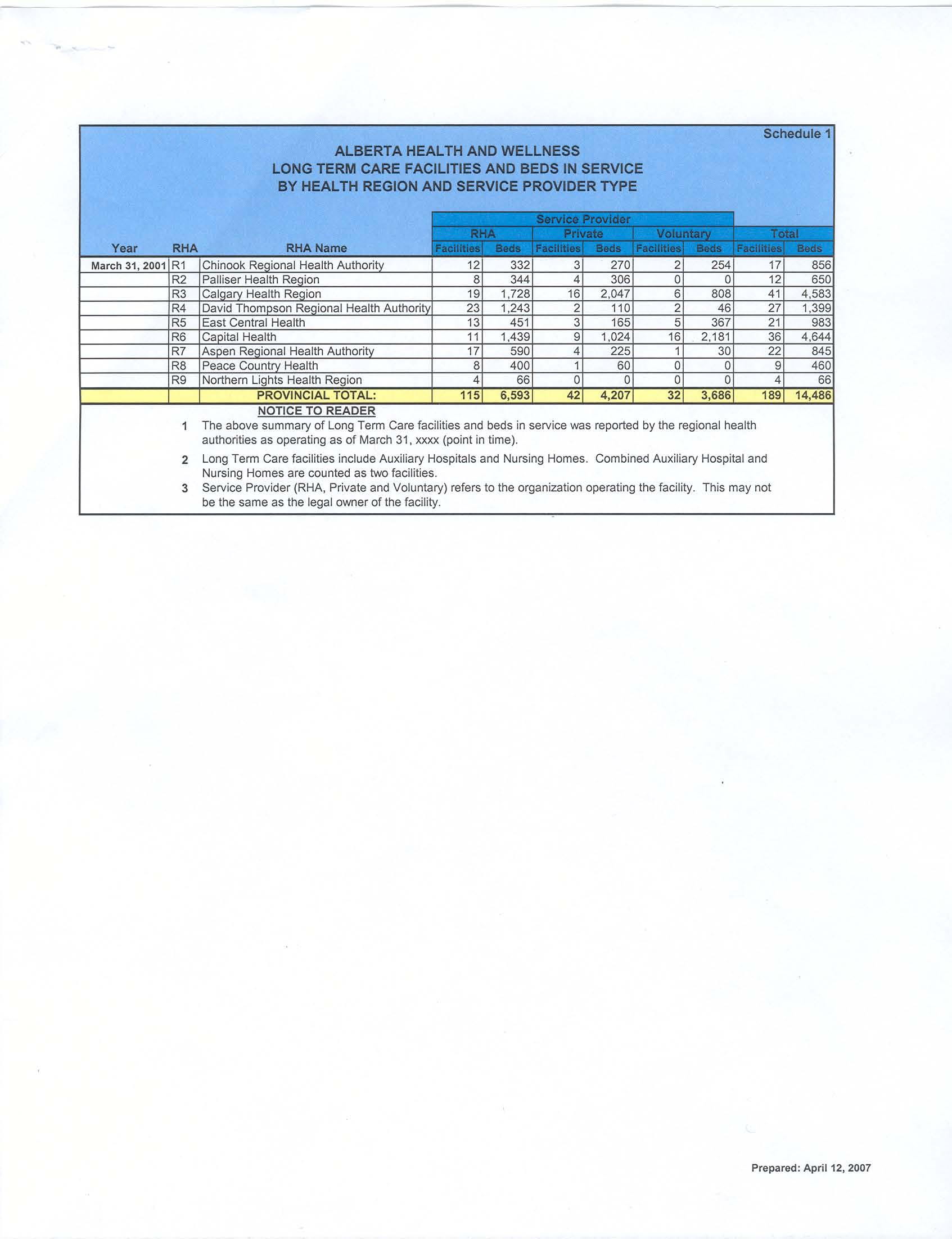
Response to Written Question WQ9, submitted May 7,2007: How many long-term care facilities and beds
were operating in Alberta on March 31 for the years 2001 to 2006 inclusive, broken down by regional
health authority and whether the facility and service providers are owned/operated publicly, privately, or
on a voluntary basis?
From File: long-term care beds by type of provider 2001-2006 as of2007.pdf;
Title: Alberta Health and Wellness Long Term Care Facilities and Beds in Service by Health Region and Service
Provider Types
Summary Chart:
AHW LONG TERM CARE FACILITIES AND BEDS, ALBERTA HEALTH AND WELLNESS; Provincial totals
Year RHA
Private Voluntary
Total
Facilities
Beds
Facilities Beds Facilities Beds Facilities Beds
2006
113
5,524
49
5,100
37
3,844
199
14,468
2005
115
5,600
47
4,825
41
3,982
203
14,407
2004
115
5,808
43
4,502
39
3,954
197
14,264
2003
117
5,745
44
4,535
35
3,783
196
14,063
2002
117
5,982
44
4,411
33
3,791
194
14,184
2001
115
6,593
42
4,207
32
3,686
189
14,486
Notes:
1. The above summary of Long Term Care facilities and beds in service was reported by the regional health
authorities as operating as of March 31,xxxx (point in time).
2. Long Term Care facilities include Auxiliary Hospitals and Nursing Homes. Combined Auxiliary Hospital and
Nursing Homes are counted as two facilities.
3. Service Provider (RHA, Private and Voluntary) refers to the organization operating the facility. This may not be the
same as the legal owner of the facility.
Comments, CW: Response provided in PDF document marked "Schedule 1"; document properties show
"Created 6/13/2007" and "Prepared April 12, 2007". Wonder what the whole document was, what other
information was in it?
These numbers don't distinguish care facility beds used for transition, respite, palliative, sub-acute, rehabilitation
& convalescence, recovery, or other short-stay purposes.
Average beds per facility: 77
2001
2006
RHA
115
6,593
113
5,524
Private
42
4,207
49
5,100
Voluntary
32
3,686
37
3,844
Total
189
14,486
199
14,468
Our Forgotten Elders: The Hidden Failings of Seniors' Care in Alberta Edmonton Journal. Edmonton, Alta.: Dec
15, 2002.
There are 174 nursing homes and auxiliary hospitals in the province with a total of 14,715 long-term care beds.
The facilities range in size from a six-bed unit in Fort Macleod to the 502-bed, multi-storey General, just west of
downtown Edmonton. Of that total:
- 6,898 beds are run by regional health authorities;
- 4,072 beds are run by private, for-profit corporations such as Extendicare;
- 3,745 beds are run non-profit organizations such as the Good Samaritan Society.
Between 1988 and 2000, as the province closed some acute-care hospitals and reconfigured others, the
number of active-treatment beds in Alberta dropped from 14,700 to about 6,400. In the past decade, more than
1,400 long-term care beds have been added and home- care programs have been expanded.
WQ10: How many supportive living facilities (including assisted living facilities, lodges, enhanced
lodges, seniors complexes, and group homes) and related number of beds were operating in Alberta for
each of the fiscal years 2001-02 to 2005-06, and for April 1, 2006 to March 19, 2007, broken down by
regional health authority and by whether the facility is owned/operated publicly, privately, or on a
voluntary basis?
The following information was taken from the Housing Information System and the Supportive Living Inventory that is
maintained by the Supportive Living and Long-Term Care Branch. Please note that the term `unit' is used instead of 'beds'.
Number of Supportive
Number of Supportive
Fiscal Year
Living Facilities
Living Units
2001l02 139*
8,005
2002/03 140*
8,182
2003104 362
18,198
2004/05 380
19,903
2005/06 390
19,934
2006/07 682
23,545
*The department tracked only publicly funded seniors' lodges prior to 2003/2004
The following information is supportive living information broken down by Regional Health Authority and by type of owner/operator far the
period of April1, 2006 - March 17, 2007.
Regional Health Private Supportive Public Supportive Voluntary Supportive
Unknown
Authority
Living
Living
Living
Facilities
Units
Facilities
Units
Facilities
Units
Facilities Units
Chinook
6
324
17 1,050
9
424
5
37
Palliser
6
446
6
509
4
562
6
34
Calgary
72
3,452
25 1,581
26
837
43
249
David Thompson
7
408
23 1,346
18
276
27
198
East Central
1
62
20
982 17
495
11
74
Capital
57
2,278
30 2,027
94
2,921
84
673
Aspen
0
0
20
996
4
101
9
78
Peace Country
2
157
14
747
0
0
15
94
Northern Lights
0
0
3
119
0
0
1
8
Total
151
7,I27
158 9,357
172
5,616
201
1,445
Comments:CW
Total facilities - 682; units 23,575; average units per facility, 35.
The number of supportive living spaces receiving public funding was reported by the Auditor General in the
2005 Seniors Report (page 44):
Designated Assisted Living Facilities 1,033 beds; other assisted living facilities 552 beds; Enhanced Lodges
307 beds; 143 lodges, with approximately 8,500 beds; and 10,000 other supportive living beds, some of which
may not have contracts with the Departments or the Regional Health Authorities to provide service.
Source: letter from the Hon. Greg Melchin, Minister Alberta Seniors and Community Supports, dated May 9, 2007
Legislative Assembly of Alberta
Title: Thursday, June 14, 2007 1:00 p.m.
Date: 07/06/14
[The Speaker in the chair]
Dr. Pannu: Thank you, Mr. Speaker. This government's enthusiasm for public health care privatization knows no
bounds. Every time they have tried to openly privatize, they have met fierce resistance on the part of an overwhelming
number of Albertans; they're proceeding nevertheless. Their latest target is long-term care. In fact, the government
has been moving to privatize long-term care for some time. It's privatization by stealth. The Conservatives know it.
They just don't want Albertans to. According to documents tabled yesterday by the Minister of Health and Wellness,
there has been a steady decrease in the number of publicly operated long-term care beds in the province and at the same
time a big increase in the privately owned . . .
The Speaker: Well, thank you, hon. member, now we'll proceed. No, no, no. I'm sorry, hon. member. Remember
we've got a rule.
Mr. Melchin: Mr. Speaker, I've obviously anticipated the question that would have been asked. We want to thank him
for the direction the government is taking to ensure that the seniors' care is there as they would desire, in the format
that they wish. Yesterday I had the opportunity, for example, of being in the Speaker's constituency at Shepherd's
Care. Certainly, this might have been a private care. This is assisted living, not necessarily long-term care, but they
have a whole range of facilities here in Edmonton also that can serve the specific needs. It doesn't even mean that you
have to transfer the place in which you live. It's a matter sometimes of providing the health to where you are rather
than having to make them move from a building to another building.
The Speaker: The hon. member.
Dr. Pannu: Thank you, Mr. Speaker. Seniors' concerns are the last thing this minister wants to address. The fact is
that from 2001 to 2006 we lost close to 11,000 (note: should be 1,000? CW) publicly run long-term care beds while the
number of privately run beds increased by over 900. Why is this government quietly squeezing out quality public
health care?
Mr. Melchin: On the contrary, we're actually working towards the direction of aging in place, allowing seniors to be
able to live in their own facilities, in their own homes to the extent that they can. Many times those in long-term care
actually even progress in health and can go back to assisted or designated assisted living. Their care and their standard
of health do change. They're not perpetually having to be in a place where they might have to die.
In respect to whether it's private or public, it has always been a combination of private. The private sector has
always participated in the provision of long-term care. That's why there's also a standard, provisions of continuing
care that have been put in place to ensure that all facilities meet the requisite high standards of patient care.
The Speaker: The hon. member.
Dr. Pannu: Thank you, Mr. Speaker. The minister knows that there are almost three times as many private supportive
living units in Calgary than there are publicly owned, and there are twice as many privately run long-term care beds in
Calgary than there are public ones. Why are seniors' lives being put at risk for the sake of a Conservative ideological
bias toward privatization at all costs?
Mr. Melchin: Well, we're certainly glad to hear the opposition put on the table that they feel that everything should be
public at all costs and that the private sector has no role in our lives. It's quite contrary to the whole development of
this great country in which we live, in which you and I can make private choices, can have private ownership and even
the provision of services to an individual that are private. In this case it is the level of care that's important and even
sustaining a person in their own place.
Summary of the Continuing Care Health Service Standards April 2007 Amendments
RHA responsibility under Continuing Care Health Service Standards May 2006, re: long term care facility residents
Notes: RHAs operate facilities and contracts with private facility operators
Issued pursuant to the authority of the Minister of Health and Wellness to issue directives and guidelines to Regional Health Authorities,
pursuant to section 8 of the Regional Health Authorities Act; replace the 1995 consolidated Basic Service Standards for Long-Term Care
Facilities. M = Mandatory requirement; P = Performance expectation.
Professional Nursing Care is not defined although it is referenced in 1.10(b).
A: Providing Quality Continuing Care Health Services
1.1
Comply with mandatory; make reasonable attempts to comply with, and to ensure contract service providers comply with,
performance expectations.
1.2
Provide general information on available services; provide relevant information to clients re: available services (P: inform clients of
known options if a specific service is not available)
1.3
Manage waitlists to provide equal opportunity for services; levels and urgency of need as prime considerations.
1.4
Provide to clients information about services provided or offered, the importance of personal directives, guardianship, trusteeship
(P), etc,; provide reasonable support for family councils (including establishing terms of reference), have a process for client
feedback and biennial surveys.
1.5
Ensure each facility has a concerns resolution process, takes reasonable steps to ensure timely response; provide clients with
information about the processes, including the HFRC, Provincial Ombudsman and PPIC.
1.6
Plan and provide health services to promote mental & physical health, independence, and the prevention of disease and injury (P).
1.7
Establish infection prevention and control guidelines and policies
1.8
Ensure that all potential clients are assessed for health service needs; if the required services or preferred setting are not available
or ideal, inform client of the risks of available services and advise of available options; If client chooses the available services or
preferred setting, work to mitigate the risks, obtain acknowledgement of the risks in writing from the client. Assess all residents by
Sept 30/07 with phase in use of the MDS 2.0 according to the AHW timeline ; complete care plans, consult with appropriate
professionals and consider the MDS protocols when preparing the care plan.
1.9
Establish policies and processes which permit client involvement in care planning.
1.10
Each client will have one care plan that includes the health service assessment; a description of the health service needs and goals
within a time frame; the service interventions that will and will not be provided or funded; the responsibilities of each health care
provider team member; how the goals will be monitored and the interventions evaluated; if expected results not achieved, a revision
of the care plan. Care plans to be reviewed/updated at least every 3 months, case conference annually; care plans to include an
evaluation of the effectiveness of the care plan; any changes to the plan or new health care service to be documented.
1.11
Establish health service coordination policies and processes, provide continuity of services, access to emergency services, identify
a case manager/coordinator who will be responsible for information to the client, ensure the assessment and care planning.
Document end-of-life wishes (P)
1.12
Ensure client health information is shared with appropriate service providers in accordance with legislation (P)
1.13
Ensure regulated health care workers work within their practice statement and competencies as defined by legislation and
professional organizations; define by policy appropriate competencies and scope of work for unregulated health care providers,
ensure they are appropriately trained and supervised to provide safe care; ensure all health care aides have graduated or
demonstrated competency in the approved curriculum by April 2008 by commencing a training program within 6 months of being
employed and completing training within 2 years.
1.14
Establish policies re: nurse practitioner services.
1.15
Ensure all clients under the care of a physician; that physicians collaborate with the medical director (P); that all facility operators
have a physician as medical director; that the medical director establish policies and procedures governing medical care of clients,
including assessments, medication review at least every 3 months; reports adverse drug reactions, and annual case conference for
each resident (P).
1.16
Establish policies and processes to ensure safe medication management, conduct an annual review of these policies, processes
and procedures (with detailed requirements for medication management responsibilities).
1.17
Assess clients for nutrition and hydrations needs using interRAI or equivalent assessment; address these needs in the care
planning process.
1.18
Where a client is assessed as requiring therapeutic services, address these needs in accordance with the care planning process;
coordinate access or referral to therapeutic services (P).
1.19 Processes to support clients in accessing services such as oral health, dental, podiatry, hearing and vision, based on assessed
health service needs (P).
1.20
Support clients in accessing medically necessary health service equipment and medical-surgical supplies where these are required
but not provided; ensure the equipment provided is in safe condition and properly used.
1.21
Establish operational policies and procedures which reflect the changing characteristics of clients and current best practice, to guide
care planning and service provision (15 areas of care services specified: e.g. care of clients with dementia, personal care of clients,
use of restraints)
B. Quality Improvement and Quality Assurance, Standards of Practice
1.22
Establish a quality improvement program to regularly evaluate and improve health care services (incorporating the HQCA Quality
Matrix: acceptability, accessibility, appropriateness, effectiveness, efficiency and safety) for the four areas of need (being healthy,
getting better, living with illness or disability and end of life.
Strive to achieve accreditation status as determined by AHW by 2010, submit annual report on same.
1.23
Collect and submit data required by the Alberta Continuing Care Information System Reporting Requirements.
1.24
Establish policies and processes to ensure compliance with the standards and relevant legislation; submit an annual report
summarizing compliance status.
Carol Wodak
What's in an hour of care?
In a 2000 newsletter, the Bethany Care Society published a basic care schedule:
24 hour care schedule for a dependent resident (total, 205 minutes, 3.42 hours)
30 minutes morning: toilet,
15 minutes help with lunch
5 minutes medication
mouth care, wash, dressing
(again, 3 - 4 people)
administration
5 minutes medications,
15 minutes 2-person
15 minutes lift onto bed, 2-
10 minutes 2-person
continence care or toilet,
person continence care or
transfer into chair
transfer /lift to bed for nap
toilet
15 minutes breakfast
10 minutes check on
15 minutes bedtime mouth
(each caregiver assisting at
resident several times;
care, wash, make
least 3 residents)
provide fluids, snacks
comfortable in bed
15 minutes assist with
10 minutes 2-person
10 minutes late evening
toileting (2-person transfer)
transfer/lift to wheelchair
check and care
10 minutes help finish off
15 minutes assistance with
10 minutes nighttime care
getting ready for the day
dinner
and comfort
The article noted that a great many every-day needs (portering to a church service,
going outside for a while, talking about family) weren't included; and the 3 hours of
funded care were expected to include: care management ( physicians' medication
orders, care conferences, care assessment and planning, calling family to update them
on changes, charting, organizing appointments and transportation, etc.); clinical care
and therapies (wound care, insulin, swallowing assessment, exercise/rehabilitation,
recreation activity, social work support, pain; control, palliation and address
unpredictable changes in clinical status); staff vacations, sick time, holidays and other
leave.
This kind of routine care schedule is fairly common, based on "time-motion" studies of
routine daily tasks for an "average" resident in actual time worked by a competent care-
giver with no distractions or other responsibilities. The discussion of appropriate "hours
of care" is simply an academic exercise without the context of the care needs of the
residents. Caring for impaired and ill people is not comparable to a controlled assembly-
line process, with discrete and predictable manual tasks.
Extract from What's in an hour of care.doc
Prospectus re purchase of CPL Dated: April 25, 1997 (Extract)
http://www.cplreit.com/Investment/Documents/APR25ENG.PDF
Document Outline
- SALT 4.doc
- 1 long term care beds by type of provider 2001_2006 summary 2.doc
- 2 long-term care beds by type of provider 2001-2006 as of2007.pdf
- ~LWF0000.pdf
- ~LWF0001.pdf
- 3 07-06-14 - qp - pannu - long-term care privatization (2).doc
- 4 Final Care Standards table.doc
- 4a Whats in an hour of care.doc
- 5 Prospectus re purchase of CPL 1997.doc